Name : P.ramyareddy
Roll no:115
Unit-1
My experience in medicine department during internship from 13/4/23 to 12/6/23
underthe guidance of dr .Lohith varma(Pgy1)
Dr.Nishita (Pgy2)
Dr.Venkat Sai (pgy2)
Dr.Zain (SR)
During these 2 months of posting I have been posted frst in
peripherals from 14/4/23 to 28/4/23 then
Unit
Psychiatry
During peripherals: 15days
First I was posted in nephrology:
I did Hrly monitoring of patients undergoing dialysis (maintanence hemodialysis)
Staging of CKD
I learnt th procedure of central line catheterisation and assisted in central line insertion
Learnt about central line care
Indications of dialysis
Complications of dialysis and their management
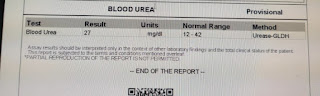
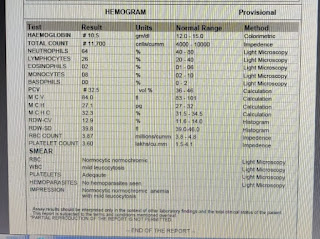
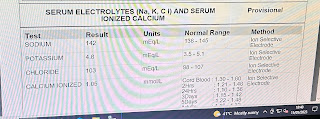
Sent post dialysis samples (CBP and RFT)
Significance of erythropoietin in CKD
Management of bradycardia during dialysis
Ward duty:
I made pajr groups and follow up for ward patients
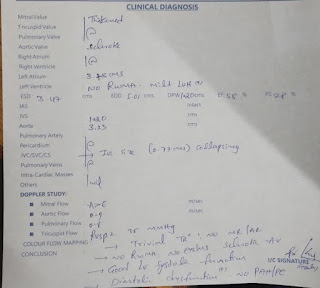
Learnt clinical examination of major systems (respiratory,CNS,CVS)
During rounds ,attended a dermatology ,psychiatry cases and a dextrocardia case which were so interesting ..
Drew blood samples and inserted cannulas
ICU AND AMC duty:
Attended rounds in ICU and AMC
Learnt how to take ABG sample and interpretation of ABG report
Assisted in LP procedure
Learnt how to do CPR in ICU
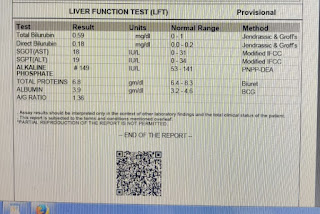
Did bladder wash for a CLD patient
Learnt about condom catheterisation
Foleys insertion
Ryles tube insertion
Did a asicitic tap for CLD pt
Learnt the difference between diagnostic and therapeutic asicitic tap
Significance of SAAG ratio and interpretation of HIGH nd low SAAG cases
Complications of ascites
Causes of Portal hypertension
Management of ascites and complications
Hepatica encephalopathy (grading and treatment)
Significance of thiamine in ALD
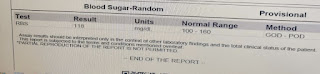
Learnt about insulin infusion rate in DKA pts
Dressings for ostemyelitis case presented with AKI
Radiological criteria of chronic pancreatitis
Wells criteria for PE
Unit duty :
Made op audit of different cases
History and examination in op
Learnt about the importance of clinical examination and coming to provisional diagnosis based on history and examination findings
Significance of Limited investigations
Counselling of patients with comorbities (DM,HTN) about diabetic diet and salt restriction diet
Learnt about basic ECG interpretation
Psychiatry duty:
Learnt about history taking in psychiatry
Learnt about schizophrenia,Alochol dependence,tobacco dependence,OCD,depressive disorder ,Generalised anxiety disorders
MSE significance
attended rounds in DAC
Counselling of psychiatry patients
Medical management of psychosis
The following links of blogs in internship period:
1) https://ramyareddy105pebbeti.blogspot.com/2023/05/65-year-old-female-with-bl-pedal-edema.html
2) https://ramyareddy105pebbeti.blogspot.com/2023/05/45-year-old-male-with-alcoholic-liver.html
3) https://ramyareddy105pebbeti.blogspot.com/2023/05/65yr-old-female-with-apd-and-ckd-stage.html
4)https://ramyareddy105pebbeti.blogspot.com/2023/05/74year-old-female-with-abdominal.html
5) https://ramyareddy105pebbeti.blogspot.com/2023/05/31year-old-male-with-acute-pancreatitis.html
6) https://ramyareddy105pebbeti.blogspot.com/2023/04/65year-old-male-with-ckd-on-mhd.html
7) https://ramyareddy105pebbeti.blogspot.com/2023/04/45-year-old-female-with-anasarca-under.html