This is online E log book to discuss our patient's deidentified health data shared after taking his/her guardian signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve the patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient centered online learning portfolio and your valuble inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of patient clinical data analysis to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
Unit -1
Ward case
DOA:15/5/23
65yr old female ,home maker ,residence of Nalgonda came with c/o abdominal distension and bloating since 4 days
HOPI: she was apparently asymptomatic 10 days ago then she developed fever ,insidious in onset,low grade ,intermittent type ,not associated with chills and Rigors ,no aggravating factors,relieving on medication,associated with body pains.
No h/o burning micturition,headache,cold and cough
C/o vomitings in these 10 days ,5-6 episode(presently had 1 episode ,with food particles as content ,non projectile ,non bilious ,non blood stained
C/o burning sensation in oral cavity since 10days(becoz of which she is unable to eat) ,no h/o dysphagia,loss of appetite and weight loss
No h/o pain abdomen ,constipation or loose stools
No h/o sob,chest pain ,pedal edema and palpitations and decreased urine output
Now since 4 days c/o abdominal distension with bloating and belching
Associated with regurgitation of food ,aggravating on lying down after taking food and no relieving factors
Past history:
K/c/o DM2 since 6 yrs on regular medication tab.vidagliptin 50mg+metformin 500mg Po/BD
HTN since 6 years on tab telma-H (40-12.5)po/OD
General examination:
Pt is conscious,coherent and cooperative well oriented to time ,place and person
Vitals :
Temp :afebrile
PR:80bpm
RR:16cpm
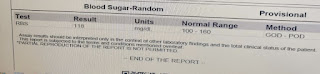
Grbs:138mg/dl
No pallor ,icterus,clubbing ,cyanosis ,lymphadenopathy,oedema
Systemic examination:
CVS:s1,s2 heard ,no murmurs
RS:BAE+,NVBS +
P/A: distended ,umbilicus :inverted
Non tender ,no organomegaly
No shifting dullness and fluid thrill
Bowel sounds +
Gastro opinion taken for endoscopy:
Impression:Atrophic fundal gastritis
opthal opinion taken I/v/o retinal changes for DM AND HTN :
Impression: on fundus examination of eye no changes of Hypertesion and diabetic retinopathy noted .
Nephrology opinion taken I/v/o deranged RFT(BU:45mg/dl and serum creatinine:1.7mg/dl)
Advised:
1.W/H tab.telma -H
2.Consider tab.cinod 10mg Po/OD
3.Consider Inj.HAI sc/TID ,
If patient is uncooperative continue same diabetic medication.
Provisional diagnosis :
APD-Acid peptic disease
Investigations:
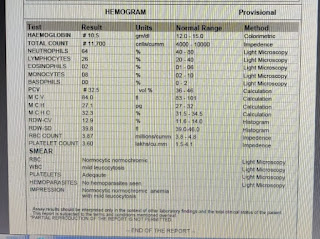
Hemogram:
RBS:
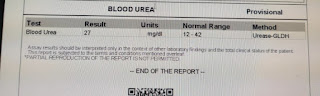
Blood urea:
Serum creatinine:
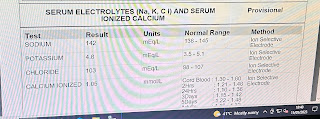
Serum electrolytes:
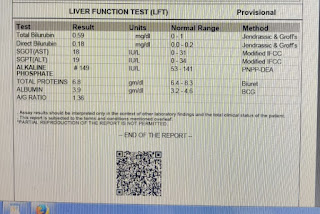
LFT
HbA1C:6.8%
CUE:
Appearance :clear
Albumin:+
Sugar :nil
Pus and epithelial cells:2-3
RBC:Nil
Serology:negative
ECG:
CXR:
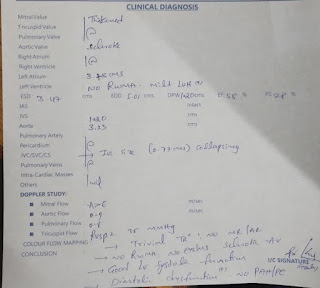
2D echo:
FINAL DIAGNOSIS:
ACID PEPTIC disease- atrophic gastritis with k/c/o HTN and DM since 6years
CKD:stage 3B
Treatment given :
1)Tab.RAZO -D 40mg Po/OD before breakfast
2)Syp.sucrafyl-o Po/TID 15mins before food
3)Tab.CINOD 10mg Po/OD
4)Tab.vidagliptin 5omg+metformin 500mg Po/BD
5)ZYTEE gel LA/TID
Advice at discharge:
1.Tab.RAZO-D 40mg Po/OD before breakfast
2.Tab.CINOD 10mg Po/OD
3.Tab.vidagliptin 5omg+metformin 500mg Po/BD
4.ZYTEE gel LA/TID
Follow up:
Review to general medicine opd after one week with RFT report