Gen med case presentation;
Jan 20,2022
Name;Ramya reddy pebbeti.
Roll no;105 .
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients’ clinical problems with collective current best evidence-based inputs. This e-log book also reflects my patient centred online learning portfolio and your valuable inputs on comment box is welcome.
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan
Following is the view of my case :
CASE PRESENTATION ;
DOA:19/01/22
chief compliants:
A 55 yr old female who is a farmer by occupation came to the opd with a chief compliants of
* Sob since 15 days
* Pedal edema since 15 days
Illness events In her life are;
8 yrs back she is diagnosed to have hypertension and she is on regular medication
5 years back she had an upper limb fracture for which she went to hospital and got treated for that and her creatinine levels were high ( from hospital reports) serum creatinine-2.8mg/dl
6 months back she tested positive for covid
5 months back her Cr level are 4.5 mg/dl
Current Cr levels are 7.9 mg/dl( on 17/01/22)
Now she came to our opd complaining of
*Sob since 15 days ( grade - 3)
*Pedal edema - since 15 days ,non pitting type
*Decreased urine output
Past history;
K/c/o HTN since 8 years
H/o taking NSAIDS for 1 year for OA ( given By a local doctor)
Personal history:
Diet- mixed
Appetite; normal
Bowel and bladder: regular
Sleep - adequate
No addictions
General examination;
Pt is conscious, coherent, cooperative and well oriented to time ,place and person
She is moderately built and moderately nourished
Pallor, clubbing , cyanosis, lymphadenopathy- absent
Edema - present ( up to ankles) and non pitting type .
Systemic examination;
RS: BAE+
CVS: S1,S2 heard
Per abdomen: soft and non tender
CNS: intact
Provisional diagnosis:
#CKD with hyperkalemia
Investigations;on 19/01/22
Hemogram:
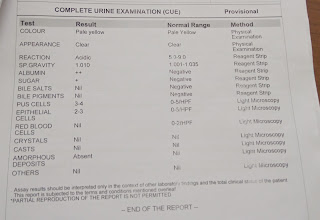
CUE;
ECG;
Treatment ; (On 20/01/22)
*Neb.with duolin
*Inj.HAI 12U
*Inj.Lasix 40mg/IV/BD
*Tab .nodosis 500 mg /po/Bd
*Tab.shelcal CT po/oD
*Tab orofer XT Po/BD
*Inj.erythropoietin 400IU/sc
*Tab.Nicardia 20 mg/po/Bd
*Strict I/O monitoring
*One round of hemodialysis on 20/01/22
And another on 22/01/22