I have been given the following cases to solve in an attmept to understand the topic of 'Patient clinical data analysis' to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and diagnosis and come up with a treatment plan.
PEBBETI RAMYA REDDY
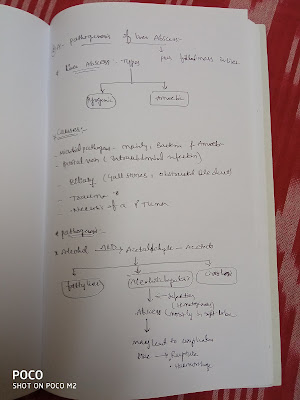
8 SEMESTER, ROLL NO; 105 .
1) Pulmonology (10 Marks)
A) Link to patient details:
Questions;
1.What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A: #symptomatology: a. SOB 30 days ago (present episode) and she had many similar episodes previously because of which she used medicines prescribed by a local RMP
b. PEDAL OEDEMA since 15 days , pitting type
c. FACIAL PUFFINESS since 15 days
#Anatomical location: LRT(bronchi, bronchioles)
#Primary etiology: usage of indoor CHULHA since 20 years
It might be due to chronic exposure to
smoke from that chulha.
2.What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A: ~Head end elevation: # MOA ;
•improves oxygenation
•decreases incidence of VAP
•increases hemodynamic performanc
•increases end Expiratory lung volume
•decreases incidence of aspiration
# Indications: •head injury
•meningitis
•pneumonia
~o2 inhalation to maintain spo2
~Bipap : non invasive method
# MOA:Assist ventilation by delivering positive expiratory and inspiratory pressure with out need for ET intubation
Usually during sleep to regulate breathing
#Indications: •COPD , VAP, OSA, BAROTRAUMA , failure of CPAP, ARDS
~ inj. Augumentin : amoxicillin +clavulanic acid
#MOA: amoxicillin- binds to PBP and inhibits bacterial
cell wall synthesis
Clavulanic acid- inactivate beta lactamase enzymes
#Indications :LRT infection, COPD, bacterial sinusitis
~ Tab. Azithromycin :macrolide antibiotic
#MOA :Inhibits bacterial protein synthesis
#Indications: CAP, PHARYNGITIS, acute exacerbation of COPD, SINUSITIS, TONSILLITIS, etc
~inj. LASIX :FUROSEMIDE - LOOP DIURETIC
#MOA :Inhibits Na - K - 2Cl COTRANSPORTER and this increase urinary excretion of sodium n water
#Indications: OEDEMA due to heart failure , RENAL FAILURE, HTN
~tab.pantop: PPI
#MOA : Binds irreversibly to
H+/K+ ATP pump and deceases acid secretion
#indication: PUD, GERD, ZES, Gastritis, to counteract the effects of steroid on GIT
~ inj. Hydrocortisone: steroid (glucorticoid analog)
#MOA: Binds to GC receptor and leads to downstream ((ANTI INFLAMMATORY)effects such as: *inhibition of Phospholipase A2, NF_kappa B,
and other inflammatory factors
#Indications: COPD, PSORIASIS, adrenal insufficiency
~ neb. Ipravent, budecort; IPRATROPIUM
BROMIDE+BUDESONIDE
#MOA: Anti Cholinergic- acts on Muscarinic receptors of bronchi _ Bronchodilation
Budesonide; steroid, anti inflammatory
#indications: • COPD, ALLERGIC RHINITIS
~Tab pulmoclear - mucolytic combination
# MOA : thins the mucus and thus which is easy to cough out
# indications ; COPD, relieve symptoms of wheezing and congestion
~ chest physiotherapy ; improves lung function
~ GRBS ;genreral random blood sugar, test to know the blood sugar levels
#indications; diabetes , prediabetes, GDM
~inj . HAI - # MOA ; Lowers blood glucose by stimulating peripheral glucose uptake by skeletal muscle and fat and inhibits hepatic glucose production
# indications: type _1 DM , DKA, TYPE 2 DM When not controlled by ORAL Anti diabetic drugs
~ vitals monitoring
~i/o charting
~inj.thiamine: it has been shown in a study that I. V thiamine increasea oxygen consumption.
#indications: *thiamine deficiency (Beri-beri), WERNICKES ENCEPHALOPATHY.
3.What could be the causes for her current acute exacerbation?
A: Might be due to exposure to allergen ( paddy husk)in her immunocompromised state or due to any infection
4.Could the ATT have affected her symptoms? If so how?
A: NO
5.What could be the causes for her electrolyte imbalance?
A; . Hyponatremia and hypocholremia might be due to Tab.TELMISARTAN ( RAAS inhibitor) r could be due to ATT.
2) Neurology (10 Marks)
A) Link to patient details:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A;~ Timeline of patient symptomatology:
*2009 (12 years ago): Started drinking alcohol
*2019 (2 years ago): Diagnosed with Diabetes Mellitus, prescribed oral hypoglycemics
*2020 (1 year ago): Has an episode of seizures (most likely GTCS)
*January 2021 (4months ago): Has another seizure episode (most likely GTCS)- following cessation of alcohol for 24 hours. Starts drinking again after seizure subsides
*Monday, May 10, 2021: Last alcohol intake, around 1 bottle. Starts having general body pains at night.
*Tuesday, May 11, 2021: Decreased food intake. Starts talking and laughing to himself. Unable to lift himself off the bed, help required.
Conscious, but non coherent. Disoriented to time, person, place.
Goes to an RMP the same day- is prescribed IV fluids and asked to visit a hospital
*Saturday, May 15, 2021: Is admitted to a tertiary care hospital for alcohol withdrawal symptoms, and is treated for the same.
~ Anatomical localisation of problem: The most probable location in the brain is the hippocampus and frontal lobe.
~ Primary etiology of patient's problem: Chronic Alcoholism
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A:
1) IVF - NS and RL
# MOA -maintains blood volume and electrolytes in the body and also provides Glucose to the body
# indications: dehydration, hypovolemic shock, to restore fluids after burns.
2) inj. Thiamine : # MOA : vitamin B1, Provides energy in deficiency conditions
# Indications: * deficient
conditions, wernickes encephalopathy, Diarrhoea, ulcerative colitis.
3) inj. Lorazepam _ Benzodiazepine
#MOA : enhances the inhibitory effects of GABA - INHIBITORY NEUROTRANSMITTER.
#indications; * anxiety disorders, panic disorders, seizures, pre operative sedation.
4) tab. Pregabalin _anticonvulsant
# MOA: binds to alpha 2 voltage gated calcium channels in cns and inhibits release of excitatory neurotransmitters
#indications ;
*partial seizures
*nerve pain
*fibromyalgia
5) inj. HAI - insulin
#MOA : reduces blood glucose levels by increasing peripheral uptake of glucose by muscle.
# Indications:
*Type 1 Dm
*uncontrollable type 2 DM
* DKA
6) Grbs; test to identify blood glucose levels
7) lactulose : artificial Dischaaride
# indications:* chronic constipation
*hepatic encephalopathy
8) inj. Kcl _ electrolytes
# MOA; prevents low blood levels of potassium
#indications ;* hypokalemia
To correct deficiency, vomiting, weakness
9) syrup potchlor- contains potassium chloride, and prevents low levels of potassium in the body
# indications;* deficiency of potassium
* electrolyte imbalance
3) Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
A; A possible cause for this is due to a phenomenon known as kindling. [1]
In kindling, repeated attempted alcohol detoxification leads to an increased severity of the withdrawal syndrome. Patients with previous withdrawal symptoms are more likely to have more medically complicated withdrawal symptoms with time.
eg, in this patient
Chronic alcohol use and kindling together leads to permanent alteration in GABA receptors, leading to downregulation of GABA. This in turn leads to inhibition of inhibitory neurotransmitter GABA, hence leading to seizures (hyperactivity).
4) What is the reason for giving thiamine in this patient?
A: One of the differential diagnoses for altered sensorium following chronic alcoholism is Wernicke-Korsakoff Syndrome, caused by deficiency of thiamine (B1). To either treat or rule this differential out, thiamine is given.
_ Thiamine is necessary to provide energy to the CNS, helps in conduction of nerve signals.
Hence, deficiency leads to confusion and ataxia, both of which are present in this patient.
5) What is the probable reason for kidney injury in this patient?
A: As the urea levels are very high, it denotes an acute onset- Acute Renal Failure.
As high serum creatinine, and urea levels are present, denotes that reabsorption from tubules is taking place- therefore the primary cause is prerenal, most probably due to generalised dehydration.
A slightly high FENa level also denotes that tubular necrosis is occurring to some degree, hence the Prerenal AKI (mostly due to dehydration) is in turn leading to Acute Tubular Necrosis (ATN).
6). What is the probable cause for the normocytic anemia?
A; Possible causes:
a. Increased oxidative stress and inflammation, leading to hemolysis of the RBCs
b. Decreased bone marrow production of RBCs, due to EPO deficiency owing to kidney failure
c. Loss of blood through chronic foot ulcer
7) Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why?
A; Yes, as alcoholism itself can cause peripheral neuropathy (alcoholic neuropathy), which along with Diabetic neuropathy, can lead to a non-healing foot ulcer.
B) Link to patient details:
Questions-
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A; ~symptomatology: *1991 - pt started consuming alcohol*13 may 2021-pt felt giddy and 1 episode of vomiting*13-16 may 2021_stopped consuming alcohol ,agin took alcohol on 16 may *17 may 2021_another bout of Giddiness , A/o with B/L aural Fullness, hearing loss, Nystagmus, 3_4 episodes of vomiting*18 may hospitalization. ~ anatomical localization: brain( CEREBELLUM and vestibular system) ~primary etiology ; might be alcohol. 2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?A; 1) Tab. Vertin- Betahistine #MOA: agonist of H1 receptor and antagonist of H3 receptor , improve the microcirculation of inner ear#indications:vertigo, tinnitus2) inj.zofer- ondansetron - ANTIEMETIC #MOA: binds to 5 HT3 receptor and thus inhibits the binding of serotonin to it . #indications: nausea and vomiting due to any cause3) Tab. Ecosprin- antiplatelet drug#MOA : low dose Aspirin prevents blood clot formation by inhibiting the action of COX enzyme# indications; *stroke * angina * heart attack4) Tab. Atorvastatin- statins #MOA :HMG CO-A reductase inhibitor, thus decrease cholesterol production in liver. #indications; *MI *STROKE*ANGINA5) BP monitoring6) Tab. Clopidogrel- antiplatelet drug#MOA: inhibits the binding of ADP to platelet P2Y12 receptor and subsequent ADP mediated activation of GP2b/3a complex, action which is irreversible. #Indications:*during PCI *ACS *Prevention of Thrombiembolism*carotid artery stenosis7) inj. Thiamine- vitamin B1#MOA:combines with ATP to produce thiamine Diphosphate , coenzyme in carb metabolism, utilization of hexose in HMP pathway. #Indications; *to correct deficiency*beri beri*neuritis8) Tab. Mvt. - vitamins and minerals #indication : to correct deficiency and anemias
3) Did the patients history of denovo HTN contribute to his current condition?A; Yes , *Decreased blood supply to that area - infarction - cerebellar infarct
*Hypertension - Atherosclerosis - Ruptures- Stroke- Cerebellar infarcts
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
A; Alcohol is a risk factor for atherosclerosis which causes - Ischemia - Ischemic stroke
C) Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?A; ~symptomatology;*2011_ quadriplegic Paralysis*oct 2020_Bilateral pedal Oedema, pitting type*10 may 2021_pain along left lowerlimb, palpitations, chest pain and heaviness, SOB _ Grade 3~anatomical localization:Peripheral nerves, LRT_ PRIMARY etiology: hypokalemia
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
A; Could be due to inadequate intake ,Transcellular shifts
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
A; Earliest change sen in ECG is decreased T wave amplitudeST depression, T wave inversion, flat Prolonged PR,Uwaves
D) Link to patient details:
QUESTIONS:
1.Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
A; seizures after ischaemic strokes. An increase in intracellular Ca2+ and Na+ with a resultant lower threshold for depolarisation, glutamate excitotoxicity, hypoxia, metabolic dysfunction, global hypoperfusion, and hyperperfusion injury
-- Seizures after haemorrhagic strokes are thought to be attributable to irritation due to (hemosideri. Deposits)caused by products of blood metabolism
-- Late onset seizures are associated with the persistent changes in neuronal excitability and gliotic scarring is most probably the underlying cause.
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
A: Initially the patient might have had Simple partial seizures (no loss of consciousness) and might have progressed to GTCS (loss of consciousness)
E) Link to patient details:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A; ~symptomatology:
*1991 - pt started consuming alcohol
*13 may 2021-pt felt giddy and 1 episode of vomiting
*13-16 may 2021_stopped consuming alcohol ,agin took alcohol on 16 may
*17 may 2021_another bout of Giddiness , A/o with B/L aural Fullness, hearing loss, Nystagmus, 3_4 episodes of vomiting
*18 may hospitalization.
~ anatomical localization: brain( CEREBELLUM and vestibular system)
~primary etiology ; might be alcohol.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A; 1) Tab. Vertin- Betahistine
#MOA: agonist of H1 receptor and antagonist of H3 receptor , improve the microcirculation of inner ear
#indications:vertigo, tinnitus
2) inj.zofer- ondansetron - ANTIEMETIC
#MOA: binds to 5 HT3 receptor and thus inhibits the binding of serotonin to it .
#indications: nausea and vomiting due to any cause
3) Tab. Ecosprin- antiplatelet drug
#MOA : low dose Aspirin prevents blood clot formation by inhibiting the action of COX enzyme
# indications;
*stroke
* angina
* heart attack
4) Tab. Atorvastatin- statins
#MOA :HMG CO-A reductase inhibitor, thus decrease cholesterol production in liver.
#indications;
*MI
*STROKE
*ANGINA
5) BP monitoring
6) Tab. Clopidogrel- antiplatelet drug
#MOA: inhibits the binding of ADP to platelet P2Y12 receptor and subsequent ADP mediated activation of
GP2b/3a complex, action which is irreversible.
#Indications:
*during PCI
*ACS
*Prevention of Thrombiembolism
*carotid artery stenosis
7) inj. Thiamine- vitamin B1
#MOA:combines with ATP to produce thiamine Diphosphate , coenzyme in carb metabolism, utilization of hexose in HMP pathway.
#Indications;
*to correct deficiency
*beri beri
*neuritis
8) Tab. Mvt. - vitamins and minerals
#indication : to correct deficiency and anemias
A; Yes ,
*Decreased blood supply to that area - infarction - cerebellar infarct
*Hypertension - Atherosclerosis - Ruptures- Stroke- Cerebellar infarcts
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
A; Alcohol is a risk factor for atherosclerosis which causes - Ischemia - Ischemic stroke
C) Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A; ~symptomatology;
*2011_ quadriplegic Paralysis
*oct 2020_Bilateral pedal Oedema, pitting type
*10 may 2021_pain along left lowerlimb, palpitations, chest pain and heaviness, SOB _ Grade 3
~anatomical localization:Peripheral nerves, LRT
_ PRIMARY etiology: hypokalemia
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
A; Could be due to inadequate intake ,Transcellular shifts
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
A; Earliest change sen in ECG is decreased T wave amplitude
ST depression, T wave inversion, flat Prolonged PR,Uwaves
D) Link to patient details:
QUESTIONS:
1.Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
A; seizures after ischaemic strokes. An increase in intracellular Ca2+ and Na+ with a resultant lower threshold for depolarisation, glutamate excitotoxicity, hypoxia, metabolic dysfunction, global hypoperfusion, and hyperperfusion injury
-- Seizures after haemorrhagic strokes are thought to be attributable to irritation due to (hemosideri. Deposits)caused by products of blood metabolism
-- Late onset seizures are associated with the persistent changes in neuronal excitability and gliotic scarring is most probably the underlying cause.
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
A: Initially the patient might have had Simple partial seizures (no loss of consciousness) and might have progressed to GTCS (loss of consciousness)
E) Link to patient details:
1) What could have been the reason for this patient to develop ataxia in the past 1 year?
A:Chronic alcoholism leads to cerebellar degeneration which caused ataxia in this patient.
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ? A; IC bleed might be due to multiple falls during binge drinking and minor head injuries which are unnoticed
# Yes, according to some studies,alcoholism leads to thiamine deficiency which inturn causes IVH ( intravascular hemorrhage) in brain, has been reported in some patients rarley OR some studies says that alcohol decreases platelet number and thus leads to bleeding OR *due to alcohol there will be falls which causes bleeding.
F) Link to patient details:
Questions
1.Does the patient's history of road traffic accident have any role in his present condition?A: yes, RTA may cause tears in BV 'S which may lead to blood clot formation which causes stroke .
2.What are warning signs of CVA?A: # sudden numbness of the face, arm or leg , especially on the one side of the body. # sudden confusion, trouble speaking or understanding # sudden trouble seeing in one r both the eyes # sudden trouble in walking, dizziness, loss of balance or coordination #sudden severe headache with no known cause.
3.What is the drug rationale in CVA?A: #antiplatelet drugs - like low dose aspirin and others like clopidogrel acts by inhibiting platelet activation # statins like atorvastatin acts by reducing blood cholesterol and thus prevents the recurrent attack of stroke
4. Does alcohol has any role in his attack?A; NO , because moderate alcohol consumption is linked to low risk of stroke.
5.Does his lipid profile has any role for his attack?A: No becoz he has normal lipid profile. As shown in report
F) Link to patient details:
Questions
1.Does the patient's history of road traffic accident have any role in his present condition?
A: yes, RTA may cause tears in BV 'S which may lead to blood clot formation which causes stroke .
2.What are warning signs of CVA?
A: # sudden numbness of the face, arm or leg , especially on the one side of the body.
# sudden confusion, trouble speaking or understanding
# sudden trouble seeing in one r both the eyes
# sudden trouble in walking, dizziness, loss of balance or coordination
#sudden severe headache with no known cause.
3.What is the drug rationale in CVA?
A: #antiplatelet drugs - like low dose aspirin and others like clopidogrel acts by inhibiting platelet activation
# statins like atorvastatin acts by reducing blood cholesterol and thus prevents the recurrent attack of stroke
4. Does alcohol has any role in his attack?
A; NO , because moderate alcohol consumption is linked to low risk of stroke.
5.Does his lipid profile has any role for his attack?
A: No becoz he has normal lipid profile. As shown in report
G) Link to patient details:
__*Questions*_
1)What is myelopathy hand ?
A; loss of power of adduction and Extension of ulnar two r three fingers and an inability to grip and release rapidly with these fingers which is due to pyramidal tract involvement.
2)What is finger escape ?
A: it is a neurological sign consisting of involuntary abduction of little finger due to unopposed action of extensor digiti minimi. Seen in cervical myelopathy.
3)What is Hoffman’s reflex?
A: it is a test to examine the reflexes of upper limb extremities
It is positive in UMN Lesions and corticospinal tract dysfunction.
H) Link to patient details:
Possible questions:
1) What can be the cause of her condition ?
A; According to MRI cortical vein thrombosis might be the cause of her seizures.
2) What are the risk factors for cortical vein thrombosis?
A;
*Infections:
_Meningitis, otitis,mastoiditis
*Prothrombotic states:
_Pregnancy, puerperium,antithrombin deficiency proteinc and protein s deficiency,Hormone replacement therapy.
*Mechanical:
_Head trauma,lumbar puncture
*Inflammatory:
_SLE,sarcoidosis,Inflammatory bowel disease.
*Malignancy.
*Dehydration
*Nephrotic syndrome
*Drugs:
_Oral contraceptives,steroids,Inhibitors of angiogenesis
*Chemotherapy:Cyclosporine and l asparginase
*Hematological:
_Myeloproliferative Malignancies
Primary and secondary polycythemia
*Intracranial :
_Dural fistula,
*venous anomalies
_Vasculitis:
_Behcets disease wegeners granulomatosis
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
A; Seizures are resolved and seizure free period got achieved after medical intervention but sudden episode of seizure was may be due to any persistence of excitable foci by abnormal firing of neurons.
4) What drug was used in suspicion of cortical venous sinus thrombosis?
A; Anticoagulants are used for the prevention of harmful blood clots.
--Clexane ( enoxaparin) low molecular weight heparin binds and potentiates antithrombin three a serine protease Inhibitor to form complex and irreversibly inactivates factor xa.
3) Cardiology (10 Marks)
A) Link to patient details:
Questions:
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
A; The amount of blood pumped out of the heart with each beat is called the ejection fraction (EF). A normal EF is usually around 55 to 70 percent, but it can be lessened in some forms of heart failure.
-People with heart failure with reduced ejection fraction (HFrEF) have an EF that is 40 to 50 percent or lower. This is also called systolic heart failure. People with heart failure with preserved ejection fraction (HFpEF) do not have much of a change in their ejection fraction. This is often called diastolic heart failure.
-HFrEF were often diagnosed earlier in life and right after a heart attack.
HFpEF were diagnosed later in life and first experienced symptoms of heart failure between the ages of 65 and 69. Many of those with HFpEF also shared that they have other health problems that led to their diagnosis. Many of them also live with additional health conditions, including acid reflux (GERD), high blood pressure, kidney disease, and sleep disorders.
-HFrEF shared that they feel depressed and/or anxious about their heart failure diagnosis. Risk factors for those in this group include genetics or a family history of heart failure.
HFpEF shared that they are still able to do the things they enjoyed before their heart failure diagnosis.risk factors, including:
- Sedentary lifestyle
- High blood pressure
- Sleep apnea
- Other heart conditions
-HFrEF are more likely to have had surgery, including surgery to implant a pacemaker or other heart rhythm control device.HFrEF shared that they currently use a combination therapy to treat their heart failure.
HFpEF have never had surgery to treat their heart failure or had a device implanted.
-HFrEF are men who live in rural areas.
However, most respondents with HFpEF are women who live in urban areas.
2.Why haven't we done pericardiocenetis in this pateint?
A: Pericardiocentesis is done when the pericardial effusion is not resolving on its own . Here the pericardial fluid which has accumulated was resolving on itw own , at the time of admission it was 2.4mm and when discharged it was 1.9 mm . Therefore we did not do pericardiocentesis in this pt.
3.What are the risk factors for development of heart failure in the patient?
A: IN THIS PATIENT:
#NON MODIFICABLE: are,
* age
* gender
#MODIFIABLE:
*hypertension
*smoking
*type 2 diabetes .
*kidney disease.
4.What could be the cause for hypotension in this patient?
A: The pt. was anemic with Hb of 8gm/dl . One of the severe complication of anemia is tissue hypoxia which further lead to hypotension..
B) Link to patient details:
Questions:
1.What are the possible causes for heart failure in this patient?
A; * obesity
*alcohol
*diabetes
* hypertension
2.what is the reason for anemia in this case?
A; Alcoholics frequently have defective red blood cells that are destroyed prematurely, possibly resulting in anemia. Alcohol also interferes with the production and function of white blood cells, especially those that defend the body against invading bacteria. Consequently, alcoholics frequently suffer from bacterial infections.
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
A; The pt. had recurrent blebs and ulcer on lower limbs (foot). This is due to Type 2 diabetes mellitus.
__ Diabetic foot ulcers generally arise as a result of poor circulation in the foot region. While high blood sugar levels and nerve damage or even wounds in the feet may result in foot ulcers in many cases.
4. What sequence of stages of diabetes has been noted in this patient?
A: alcohol------obesity------impaired glucose tolerance------diabetes mellitus------microvascular complications like triopathy and diabetic foot ulcer-------macrovascular complications like CAD, PVD.
C) Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A;~symptomatology;
*SOB - grade 2 to grade progressed
* decreased urine output since 2 days.
~ the anatomical site is BLOOD VESSELS;
~ ETIOLOGY:
_ The physical stress of hypertension on the arterial wall also results in the aggravation and acceleration of atherosclerosis, particularly of the coronary and cerebral vessels. Moreover, hypertension appears to increase the susceptibility of the small and large arteries to atherosclerosis.
The most likely cause of arterial thrombosis is artery damage due to atherosclerosis. Atherosclerosis occurs when a person has a buildup of plaque on the walls of their arteries. The arteries then begin to narrow and harden, which increases a person's risk of developing arterial thrombosis.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A : PHARMACOLOGICAL INTERVENTIONS
1. TAB. Dytor
MOA; Through its action in antagonizing the effect of aldosterone, spironolactone inhibits the exchange of sodium for potassium in the distal renal tubule and helps to prevent potassium loss.
2. TAB. Acitro
MOA: Acenocoumarol inhibits the action of an enzyme Vitamin K-epoxide reductase which is required for regeneration and maintaining levels of vitamin K required for blood clotting
3. TAB. Cardivas
MOA: Carvedilol works by blocking the action of certain natural substances in your body, such as epinephrine, on the heart and blood vessels. This effect lowers your heart rate, blood pressure, and strain on your heart. Carvedilol belongs to a class of drugs known as alpha and beta-blockers
4. INJ. HAI S/C :
#MOA; Regulates glucose metabolism
Insulin and its analogues lower blood glucose by stimulating peripheral glucose uptake, especially by skeletal muscle and fat, and by inhibiting hepatic glucose production; insulin inhibits lipolysis and proteolysis and enhances protein synthesis; targets include skeletal muscle, liver, and adipose tissue
# INDICATIONS; TYPE 1 DM, DKA
5.TAB. Digoxin
#MOA; Digoxin has two principal mechanisms of action which are selectively employed depending on the indication:
Positive Ionotropic: It increases the force of contraction of the heart by reversibly inhibiting the activity of the myocardial Na-K ATPase pump,
an enzyme that controls the movement of ions into the heart.
6. Hypoglycemia symptoms explained
7. Watch for any bleeding manifestations like Petechiae, Bleeding gums.
8. APTT and INR are ordered on a regular basis when a person is taking the anticoagulant drug warfarin to make sure that the drug is producing the desired effect.
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
A;*cardiorenal syndrome type 4 is seen in this patient.
4) What are the risk factors for atherosclerosis in this patient?
A;effect of hypertention,
They can also impair blood vessels' ability to relax and may stimulate the growth of smooth muscle cells inside arteries. All these changes can contribute to the artery-clogging process known as atherosclerosis.
5) Why was the patient asked to get those APTT, INR tests for review?
A; APTT and INR are ordered on a regular basis when a person is taking the anticoagulant drug warfarin to make sure that the drug is producing the desired effect.
Here, an INR of 3-4.5 is recommended. Warfarin should be started in conjunction with heparin or low molecular weight heparin when the diagnosis of venous thromboembolism is confirmed, although local protocols may vary in their starting doses and titration schedule.
D) Link to patient details:
Questions;
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A: # symptomatology;
* h/o of heartburn like episodes since one year
*H/o TB diagnosed 7 months ago and completed her course of treatment
*SOB since 1/2 hour prior to hospitalization
# anatomical localization: BLOOD VESSELS.
# primary etiology: she has h/o HTN And DM which are the risk factors for development of plaque in BV'S and thus leading to angina or atherosclerosis.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A; ~ Tab. MET XL - metoprolol
#MOA: it is a cardioselective beta blocker, and thus it reduces hear rate, BP, and cardiac output. It also lowers the risk of recurrent attacks of angina /MI.
# indications; ANGINA, MI, HTN, STROKE.
~ PCI : non surgical procedure _ angioplasty with stent placement in bV'S of heart that has been blocked by plaque formation.
3) What are the indications and contraindications for PCI?
# indications;
*Angina ( both stable and unstable)
* STEMI
* NON ST elevation acute coronary syndrome.
# C/I :
*Hyper coagulable state
* absence of cardiac surgery backup
* high garde CKD
*AN artery with a diameter of less than 1.5 mm
4) What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on overtesting and overtreatment important to current healthcare systems?
A;although the pci is safe, it has some complications like
*allergic reaction to contrast dye
* bleeding
* damage to BV'S
*requirement of emergency CABG. Becoz of this complications it is better to avoid PCI in patients who do not require it.
E) Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A;
1) ~symptamatology;
*chest pain since 3 days
*profuse sweating and Giddiness since 1 day
~anatomical localization: BV'S of heart
~primary etiology; presence of risk factors like HTN AND DM which leads to ATHEROSCLEROSIS
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A: pharmacological ;
~Tab. Aspirin-ANTICOAGULANT
(low dose)
#MOA: COX inhibitor, resulting in inhibition of platelet aggregation
#indications; angina, Stroke, MI
~ Tab. Atorvas - STATIN
#MOA: HMG _CO-A Reductase inhibitor and thus decreases cholesterol productiom in liver.
#indications:
*MI, Stroke, Angina
~Tab.clopibb _ antiplatelet drug
#MOA:inhibits binding of ADP to platelet P2Y12 receptor and subsequent ADP mediated activation of GP 2b/3a complex , thus inhibits platelet aggregation.
#Indications: *PCI , ACS, prevention of Thrombiembolism, carotid artery stenosis.
~inj, HAI - INSULIN
#MOA: reduces blood glucose by increasing peripheral uptake of glucose by muscle.
#indications: Type 1 DM
Type 2 DM, DKA
~ vital monitoring.
Non pharmacological;
#PTCA _procedure to restore the blood flow through the artery.
Types; *balloon angioplasty
*coronary stent
*atherectomy
*laser angioplasty
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
A; second PCI was not necessary In this patient .
PCI performed from 3-28 Days after MI does not decrease the incidence of death , reinfarction or NYHA Class 4 heart failure
But it is associated with Higher rates ofBoth procedure related and true st elevation reinfarction. A retrospective analysis of the clinical Data revealed the thrombolysis in MI risk score of 4 predicting a 30 day Morality of 7.3%In this patient.late PCI leads to the increased risk of periprocedural complications, long-term bleeding And stent thrombosis.
F) Link to patient details:
Questions;
1. How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
A; Because of the fluid lossoccured to the patient
There is
Decreased preload → SOB occured due to decreased cardiac output
IV fluids administered → there is increase in preload → SOB decreased due to better cardiac output
2. What is the rationale of using torsemide in this patient?
A: Torsemide is used due to abdominal distension
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
A; rationale - used for any bacterial infection .
4) Gastroenterology (& Pulmonology) 10 Marks
A) Link to patient details:
QUESTIONS:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A;
~ symptomatology :
*5 years back-1st episode of pain abdomen and vomitings
Stopped taking alcohol for 3 years
*1 year back 5 to 6 episodes of pain abdomen and vomitings after starting to drink alcohol again
*20 days back increased consumption of toddy intake
*Since 1 week pain abdomen and vomiting
*Since 4 days fever constipation and burning micturition
~Anatomical localisation: Pancreas and left lung
~ etiology; Alcohol and its metabolites produce changes in the acinar cells, which may promote premature intracellular digestive enzyme activation thereby predisposing the gland to autodigestive injury. Pancreatic stellate cells (PSCs) are activated directly by alcohol and its metabolites and also by cytokines and growth factors released during alcohol-induced pancreatic necroinflammation. Activated PSCs are the key cells responsible for producing the fibrosis of alcoholic chronic pancreatitis
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
A;
1) ING. MEROPENAM ; TID for 7 days
* Meropenem ( broad spectrum Carbepenem ) an antibiotic.
2) ING. METROGYL 500 mg IV TID for 5 days
* inj. Metrogyl has METRONIDAZOLE
( Nitroimidazole drug ) an antibiotic
3) ING. AMIKACIN 500 mg IV BD for 5days
* It is an Aminoglycoside antibiotic
## Here all three of these (Inj. Meropenem, Inj. Metrogyl, Inj. Amikacin ) are used as antibiotics to control infection and ; to prevent septic complications of acute pancreatitis.
4) TPN ( Total Parenteral Nutrition )
* Method of feeding that by passes gastrointestinal tract
* Fluids are given to vein , it provides most of the nutrients body needs.
* TPN has proteins, carbohydrates, fats, vitamins, minerals.
5) IV NS / RL at the rate 12l ml per hour
* Given for fluid replacement ie., treat dehydration
6) ING. OCTREOTIDE 100 mg SC , BD
* It is a Somatostatin long acting analogue.
* It is used here to decrease exocrine secretion of pancreas and it also has anti- inflammatory & cytoprotective effects.
7) ING. PANTOP 40 mg IV , OD
* Inj. Pantop has PANTOPRAZOLE ( Proton Pump Inhibitor) used for its anti pancreatic secretory effect.
8) ING. THIAMINE 100 mg in 100 ml NS IV , TID
* It is B1 supplement.
* It is given here because; due to long fasting & TPN usage , body may develop B1 deficiency
* Wernicke encephalopathy secondary to B1 deficiency may be caused... so a prophylactic B1 supplemention is necessary.
9) ING. TRAMADOL in 100 ml NS IV , OD
* It is an opioid analgesic, given to releive pain.
B) Link to patient details:
Questions;
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
A; the cause of dyspnea might be PLEURAL EFFUSION
A; *This hyperglycemia could thus be the result of a hyperglucagonemia secondary to stress
* the result of decreased synthesis and release of insulin secondary to the damage of pancreatic β-cells
* elevated levels of catecholamines and cortisol
3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
A; LFT are increased due to hepatocyte injury
*If the liver is damaged or not functioning properly, ALT can be released into the blood. This causes ALT levels to increase. A higher than normal result on this test can be a sign of liver damage.
*elevated alanine transaminase (ALT) and aspartate transaminase (AST), usually one to four times the upper limits of normal in alcoholic fatty liver.
The reasons for a classical 2:1 excess of serum AST activity compared to serum ALT activity in alcoholic hepatitis have been attributed to
(i) decreased ALT activity most likely due to B6 depletion in the livers of alcoholics
(ii) mitochondrial damage leading to increased release of mAST in serum.
4) What is the line of treatment in this patient?
A; Plan of action and Treatment:
Investigations:
✓ 24 hour urinary protein
✓ Fasting and Post prandial Blood glucose
✓ HbA1c
✓ USG guided pleural tapping
Treatment:
• IVF: 125 mL/hr
• Inj PAN 40mg i.v OD
• Inj ZOFER 4mg i.v sos
• Inj Tramadol 1 amp in 100 mL NS, i.v sos
• Tab Dolo 650mg sos
• GRBS charting 6th hourly
• BP charting 8th hourly
For the master chart to the "pancreatitis thesis project" please get in touch with Dr Shashikala PGY1 and Dr Divya PGY2 and share their insights into the above project problem they are working on.
C) Link to patient details:
Possible Questions :-
1) What is the most probable diagnosis in this patient?
(Differential Diagnosis:
A; * Ruptured Liver Abscess.
*Organized collection secondary to Hollow viscous Perforation.
*Organized Intraperitoneal Hematoma.
*Free fluid with internal echoes in Bilateral in the Subdiaphragmatic space.
*Grade 3 RPD of right Kidney
(The most probably diagnosis is there is abdominal hemorrhage. This will give reasoning to the abdominal distention, and the blood which is aspirated.
2) What was the cause of her death?
A; (After leaving the hospital, the patient went to Hyderabad and underwent an emergency laparotomy surgery. The patient passed away the next day. Cause of her death can be due to complications of laparotomy surgery such as, hemorrhage (bleeding), infection, or damage to internal organs.
3) Does her NSAID abuse have something to do with her condition? How?
A; (NSAID-induced renal dysfunction has a wide spectrum of negative effects, including decreased glomerular perfusion, decreased glomerular filtration rate, and acute renal failure. Chronic NSAIDs use has also been related to hepatotoxicity. While the major adverse effects of NSAIDs such as gastrointestinal mucosa injury are well known, NSAIDs have also been associated with hepatic side effects ranging from asymptomatic elevations in serum aminotransferase levels and hepatitis with jaundice to fulminant liver failure and death.
5) Nephrology (and Urology) 10 Marks
A) Link to patient details:
Questions;
1. What could be the reason for his SOB ?
A; it might be due to POST TURP SYNDROME,as SOB is the component of this syndrome.
2. Why does he have intermittent episodes of drowsiness ?
A; absorption of large volumes of irrigation fluid during TURP can produce HYPONATREMIA which causes episodes of drowsiness.
3. Why did he complaint of fleshy mass like passage in his urine?
A; it might be due to large number of pus cells?
4. What are the complications of TURP that he may have had?
A; urinary retention,, UTI.
B) Link to patient details:
Questions;
1.Why is the child excessively hyperactive without much of social etiquettes ?
A: Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by inattention, or excessive activity and impulsivity, which are otherwise not appropriate for a person's age
For a diagnosis, the symptoms have to be present for more than six months, and cause problems in at least two settings (such as school, home, work, or recreational activities).
2. Why doesn't the child have the excessive urge of urination at night time ?
A; Since the child doesn’t have excessive urge of urination at night but at day there might be a psychiatry related condition
1. Psychosomatic disorder
2. Undiagnosed anxiety disorder
3. How would you want to manage the patient to relieve him of his symptoms?
A; bacterial kidney infection, the typical course of treatment is antibiotic and painkiller therapy.
-- If the cause is an overactive bladder, a medication known as an anticholinergic may be used. These prevent abnormal involuntary detrusor muscle contractions from occurring in the wall of the bladder
* To treat attention deficit hyperactivity disorder:
For children 6 years of age and older, the recommendations include medication and behavior therapy together — parent training in behavior management for children up to age 12 and other types of behavior therapy and training for adolescents. Schools can be part of the treatment as well.
#Methylphenidate A stimulant and a medication used to treat Attention Deficit Hyperactivity Disorder. It can make you feel very ‘up’, awake, excited, alert and energised, but they can also make you feel agitated and aggressive. They may also stop you from feeling hungry.
# Amphetamine belongs to a class of drugs known as stimulants. It can help increase your ability to pay attention, stay focused on an activity, and control behavior problems. It may also help you to organize your tasks and improve listening skills.
6) Infectious Disease (HI virus, Mycobacteria, Gastroenterology, Pulmonology) 10 Marks
A) Link to patient details:
Questions:
1.Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
A; # clinical history pointing towards TEF are *initial non productive cough, difficulty in swallowing, Hoarsness of voice, RVD positive ( might be due to Opportunistic candidal infection in RVD patients).
# Physical fundings: * bilateral wheeze,( in mammory areas) and positive laryngeal crepitus.
# Physical fundings: * bilateral wheeze,( in mammory areas) and positive laryngeal crepitus.
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
Ans ; IRIS, development of which depends on CD4 COUNT of the patient , as shown in below link ,
https://dermnetnz.org/topics/immune-reconstitution-inflammatory-syndrome/
* Yes we can prevent it by careful monitoring of patients with HIV with low CD4 COUNT and thorough history of coinfections and most effective measure would be initiation of ART before development of advanced immunosuppression.
7) Infectious disease and Hepatology:
A)Link to patient details:
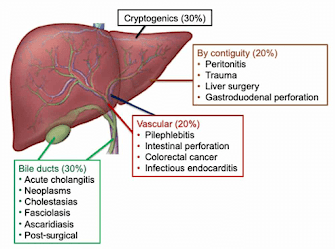
1. Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors
present in it ?
A: yes, it could be due to consumption of contaminated toddy.
2. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
3. Is liver abscess more common in right lobe ?
A: yes becoz it receives more blood supply from superior mesenteric and portal system, streaming effect in portal circulation is causative.
4.What are the indications for ultrasound guided aspiration of liver abscess ?
A: left lobe abscess >10 CM in diameter
Impending rupture
Abscess that do not respond to medical therapy .
B) Link to patient details:
QUESTIONS:
1) Cause of liver abcess in this patient ?
A: The patient is occasional toddy drinker which has high amount of Entamoeba histolytica. This causes liver abscess by suppressing the function of Kuffper cells.Therefore Toddy is most probable cause of Liver abscess in this patient
2) How do you approach this patient ?
A; Hematology:
*Common hematological finding being LEUCOCYTOSIS , indicating inflammation or infection.
* Anemia may be present , or not.
Chemistry:
* Elevated liver enzymes such as AST,ALP are noted .
3) Why do we treat here ; both amoebic and pyogenic liver abcess?
A; INJECTION. ZOSTUM 1.5 gm IV BD (twice daily)
Zostum is a combination of drugs - SULBACTUM (pencillin) & CEFOPERAZONE(cephalosporin) [Antibiotic]: It is used here to treat if any bacterial cause ( since we can’t take the risk relying on only anti amoebic therapy)
* INJECTION. METROGYL 500mg IV TID ( thrice daily )
Metrogyl has the drug called METRONIDAZOLE[Antibiotic]: For amoebic cause
* INJECTION. OPTINEURIN 1amp in 100 ml NS( Nor
mal Saline) IV OD ( once daily)
_ Optineurin is a multivitamin drug { A combination of B1,B2, B3, B5,B6, B12 } given here as a supplement
* TAB. ULTRACET 1/2 QID( four times a day)
Ultracet is a combination of drugs - TRAMADOL(opiod analgesic) and ACETAMINOPHEN (analgesic and antipyretic) : Given for pain and fever
* TAB. DOLO 650 mg SOS (if needed) given for fever and pain
* Here ; due to medical therapy his symptoms subsided and clearly we can see it in usg reports ( liquefaction) meaning abcess responded to our medical therapy.
*And the patient was discharged on 10/5/21.
* We donot aspirate the pus since it is self resolving and aspiration is associated with several other complications.
4) Is there a way to confirmthe definitive diagnosis in this patient?
A; Apart from serological examination which is positive in 94% of the cases..Further confirmation can be done by using Ultrasonography but these are not commonly used
8) Infectious disease (Mucormycosis, Ophthalmology, Otorhinolaryngology, Neurology) 10 Marks
A) Link to patient details:
Questions :
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A; * 3 years ago- diagnosed with hypertension
* 21 days ago- received vaccination at local PHC which was followed by fever associated with chills and rigors, high grade fever, no diurnal variation which was relieved on medication
* 18 days ago- complained of similar events and went to the the local hospital, it was not subsided upon taking medication(antipyretics)
*11 days ago - c/o Generalized weakness and facial puffiness and periorbital oedema. Patient was in a drowsy state
*4 days ago-
•patient presented to casualty in altered state with facial puffiness and periorbital oedema and weakness of right upper limb and lower limb
•towards the evening patient periorbital oedema progressed
•serous discharge from the left eye that was blood tinged
was diagnosed with diabetes mellitus
patient was referred to a government general hospital
•• patient died 2 days ago
patient was diagnosed with diabetic ketoacidosis and was unaware that he was diabetic until then. This resulted in poorly controlled blood sugar levels. The patient was diagnosed with acute oro rhino orbital mucormycosis . rhino cerebral mucormycosis is the most common form of this fungus that occurs in people with uncontrolled diabetes ( https://www.cdc.gov/fungal/diseases/mucormycosis/definition.html ) the fungus enters the sinuses from the environment and then the brain.
The patient was also diagnosed with acute infarct in the left frontal and temporal lobe. Mucormycosis is associated with the occurrence of CVA ( https://journal.chestnet.org/article/S0012-3692(19)33482-8/fulltext#:~:text=There%20are%20few%20incidences%20reported,to%20better%20morbidity%2Fmortality%20outcomes. )
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
A; The proposed management of the patient was –
# inj. Liposomal amphotericin B according to creatinine clearance
#200mg Iitraconazole was given as it was the only available drug which was adjusted to his creatinine clearance
# Deoxycholate was the required drug which was unavailable
https://pubmed.ncbi.nlm.nih.gov/23729001/ this article talks about the efficacy and toxicity of different formulations of amphotericin B
along with the above mentioned treatment for the patient managing others symptoms is also done by-
~ Management of diabetic ketoacidosis – :
# Fluid replacement- The fluids will replace those lost through excessive urination, as well as help dilute the excess sugar in blood.
# Electrolyte replacement-The absence of insulin can lower the level of several electrolytes in blood. Patient will receive electrolytes through a vein to help keep the heart, muscles and nerve cells functioning normally.
# insulin therapy- Insulin reverses the processes that cause diabetic ketoacidosis. In addition to fluids and electrolytes, patient will receive insulin therapy
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
A; Mucormycosis is may be being triggered by the use of steroids, a life-saving treatment for severe and critically ill Covid-19 patients. Steroids reduce inflammation in the lungs for Covid-19 and appear to help stop some of the damage that can happen when the body's immune system goes into overdrive to fight off coronavirus. But they also reduce immunity and push up blood sugar levels in both diabetics and non-diabetic Covid-19 patients.
With the COVID-19 cases rising in India the rate of occurrence of mucormycosis in these patients is increasing.
9) Infectious Disease (Covid 19)
As these patients are currently taking up more than 50% of our time we decided to make a separate log link here:
for this question that contains details of many of our covid 19 patients documented over this month and we would like you to:
1) Sort out these detailed patient case report logs into a single web page as a master chart
2) In the master chart classify the patient case report logs into mild, moderate severe and
3) indicate for each patient, the day of covid when their severity changed from moderate to severe or vice versa recognized primarily through increasing or decreasing oxygen requirements
4) Indicate the sequence of specific terminal events for those who died with severe covid (for example, altered sensorium, hypotension etc).